Patient funding alternative programs can also affect the member’s experience. The process of having coverage denied, applying for aid, and waiting to see if funds are available takes time.
A member may go through the process only to find they’re ineligible for needs-based funding because they earn too much. Or, perhaps they are eligible, but all of the program’s funding has already been used.10
Clinical risk
Treatment delays can have very serious consequences. For example, when cancer treatments — including chemotherapy — are delayed even 1 month, patients have up to a 13% higher risk of death. That risk keeps rising the longer their treatment is delayed.11
When or if the patient must be transferred back to their original coverage, there’s another risk for delayed care. The transfer process takes time, posing a serious risk of a gap in therapy. And the patient may suddenly incur out-of-pocket costs they're not prepared for.
Finally, specialty patients often have many medical needs. For example, rheumatology patients commonly have 3 or more chronic conditions.12 These patients need careful management to coordinate care, prevent waste, and monitor drug dose, site selection, and medication adherence and response.
Clinical management programs are a core value provided by a full-service PBM like Optum Rx. Our systematic, end-to-end specialty drug management includes cost and clinical management from the point of prescribing to dispensing, through first use and throughout treatment. This strategy offers better value through holistic, coordinated care.
Ethical and legal considerations
Some alternative funding programs carry potentially harsh consequences for both plan sponsors and members. But consider the ethical issues:
- Charity funds and manufacturer assistance programs are intended for patients who don’t have insurance coverage. These funds play a vital role.
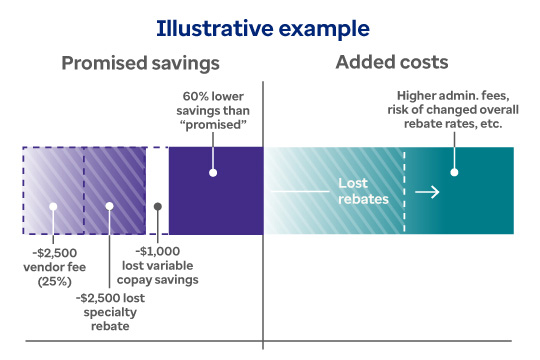
- Alternative funding vendors can charge payers up to 25% of the savings they achieve. But this means diverting critically needed funds away from uninsured patients.
- The inevitable result is less money for uninsured patients while the alternative funding vendors profit. It's an ethical dilemma that puts patient access to needed care at risk.
Ethical concerns can also become potential legal concerns as well.
Industry observers believe some funding alternatives could introduce discrimination risk into a client’s benefit structure. Self-insured plans could face ERISA and IRS compliance issues.13
Some alternative funding vendors will try to source needed drugs from a foreign market if they can’t secure funding through a patient assistance program.14 Foreign sourcing for prescription drugs is an intricate area of the law. Plan sponsors may want to seek additional guidance to avoid complications. Also, these international programs generally ship 90 days of high-cost specialty medication at a time, which increases the chance of waste.
Additionally, alternative funding vendors usually require individual members to sign a patient authorization form. The form certifies that they’re not enrolled in a healthcare program that pays for any part of their prescription drug costs.15
Consider nontraditional funding sources with caution
An online search for alternative funding programs typically presents them in a positive way — if they aren’t outright sales pitches.16 But some alternative funding schemes cause more problems than they’re worth. Anyone thinking about an alternative funding program should consider this option carefully.
For example, ask:
- What happens when the alternative funding ends or runs out?
- How will my plan afford these medications when they suddenly need to be funded again?
At Optum, we encourage longer-term and sustainable strategies over short-term solutions that can pose financial and regulatory risks. We strongly urge our clients to look past the short-term sales pitch and consider longer-term financial implications, compliance risk and ethics of alternative funding programs.
Contact your consultant or Optum representative to learn more about your options.