Last year we wrote about the problem of “vaccine fatigue,”1 which can cause some people to simply tune out vaccination campaigns — not just for COVID-19, but also for the flu.2
This fall there will be yet another round of vaccination decisions to make. In addition to updated vaccines for COVID-19 and the flu, many Americans will be eligible for new vaccines to prevent Respiratory Syncytial Virus (RSV).3 Experts are worried that vaccine fatigue may once again be a barrier to widespread vaccination.4
Fortunately, research has shown how to position vaccination to make it more appealing. Positive emotional messages like altruism, happiness and hope are the most effective way to encourage vaccination.5
The reason this works has to do with how we think about life’s challenges. Some people believe that their health is mainly controlled by outside forces — things like fate, chance or genetics. And to some degree this can be true.6
But others believe that health is something that is largely in their own power to control.7 Another term for this is “agency.”8
People who believe that we can control our health often experience more favorable health outcomes and psychological well-being than those who don’t.9
The feeling of agency and control in life is something that can be strengthened with use.10 Vaccination is one of the concrete steps we can take to reinforce our sense of agency and control.11
We do need to recognize that people can have a variety of reasons to not be vaccinated. The same messages won’t work for everyone.12
With these caveats, research on vaccination messaging has found several themes that have been proven effective. While some of these themes can overlap, here we have grouped them as positive, protection and community messages.
[NOTE: This article is for informational purposes only. It is not intended as medical advice. Anyone who has questions or concerns about getting either a flu vaccine or a COVID-19 vaccine should consult their care provider.]
1. Positive emotional messages
Positive emotional messages include feelings like altruism, happiness and hope.13
Focusing on the positive is not the same as ignoring the problem. For one thing, there really is tremendously good news to share about vaccinations.14
A hopeful or optimistic approach might start by recalling that historically vaccination has saved more lives than any single factor except sanitary drinking water.15
- Smallpox was completely eradicated by vaccination in 1977. In the 77 years prior, smallpox caused between 300–500 million deaths worldwide.16
- Worldwide, immunization now prevents up to 5 million deaths every year from diseases like diphtheria, tetanus, pertussis, influenza and measles.17
Vaccines for COVID-19 are another success story. Scientists were able to deliver a safe and effective vaccine in less than one year. (The previous record was four years.)18
The long success story of vaccination is certainly a cause for optimism.
2. Protection messages
Many people respond well to messages about protecting themselves and their loved ones against severe disease.19 A study conducted shortly after the first COVID-19 vaccines became available showed “self-protection” as the second highest ranked reason why people agreed to be vaccinated.20
So, while it may seem obvious, it never hurts to remind ourselves just how effective our vaccines really are.
Vaccination is a strong, positive action that virtually anyone can take to protect themselves against disease. That should go a long way towards making us happier and more hopeful.
COVID-19 vaccines saved 280,000 lives
This graphic illustrates what could have happened without a widespread vaccination program for COVID-19.

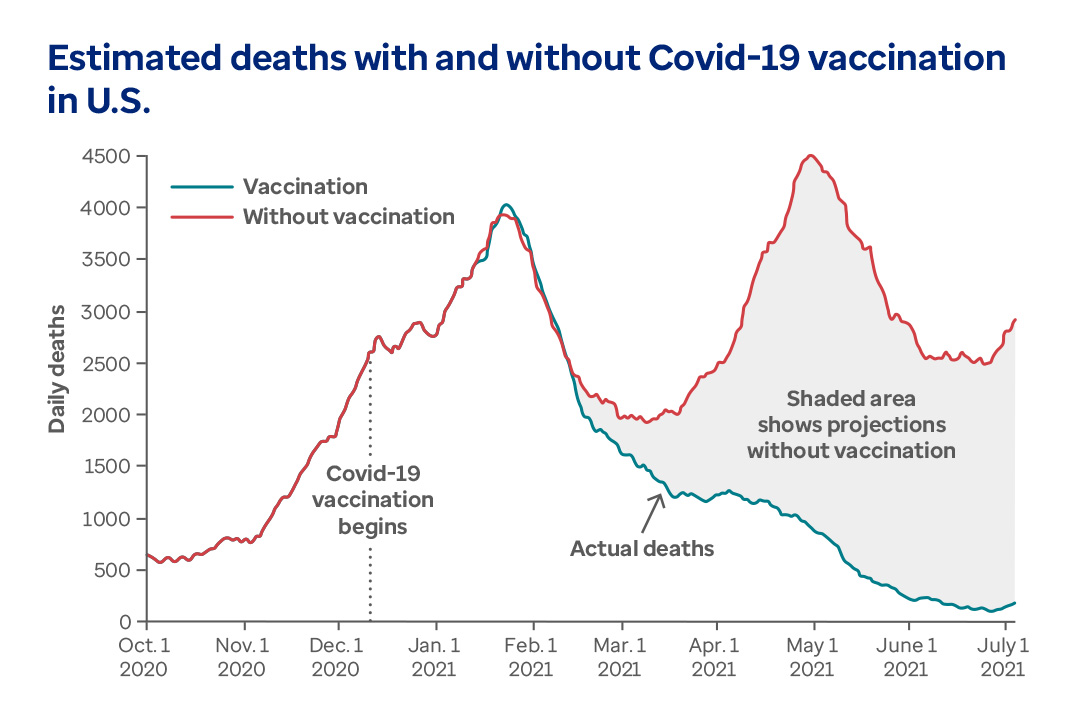
[Image adapted from Commonwealth Fund. Deaths and Hospitalizations Averted by Rapid U.S. Vaccination Rollout. Published July 7, 2021.]
Vaccination is a strong, positive action that virtually anyone can take to protect themselves against disease. That should go a long way towards making us happier and more hopeful.
[Image adapted from Commonwealth Fund. Deaths and Hospitalizations Averted by Rapid U.S. Vaccination Rollout. Published July 7, 2021.]
3. Community messages
When a wave of pandemic illness strikes, we can see the impact on the whole society. Widespread sick days, interrupted production schedules and overwhelmed hospitals are just some of the effects.21
In addition to protecting health, vaccination provides a broad array of benefits to society.22
For example, people report a sense of personal altruism and community spirit from getting a vaccine in times of crisis.23 A recent study found that the number one reason given to accept the COVID-19 vaccine was, “It is a social duty to protect my community.”24
But there are many other benefits of vaccination. For example, one of the biggest health care crises today is the increasing threat of antibiotic resistance.25 The CDC estimates that antibiotic resistance kills approximately 36,000 Americans of all ages per year. Of these, nearly 12,000 are adults aged 65 and over.26
One of the most important steps we can take to slow the spread of antibiotic resistance is to prevent the overuse of antibiotics in the first place. According to the CDC, preventing infection through vaccination reduces the need to treat infections with antibiotics.27
Vaccination can also help contribute to other social values such as herd immunity and health equity.
Herd immunity means getting vaccinated to protect people who can’t protect themselves. These include infants, the elderly, pregnant women and patients with chronic illnesses.28
We also know that health disparities exist across a range of factors like race, sex, education and income. These disparities include infection rates for communicable disease. Broadly applied vaccination programs can help level the health risks related to many under-resourced communities.29
What the future holds for promoting vaccinations
Part of keeping a positive outlook about vaccination means having realistic expectations.
COVID-19, the flu and RSV are all caused by viruses. Viruses are in some ways mysterious — it’s not even clear whether they are actually alive.30
But what we do know is that viruses have a lot of genetic variability. That gives them an amazing ability to adapt and survive. In fact, they may well be the most successful inhabitants of Earth.31
Without a historic scientific breakthrough, we may need periodic vaccinations for one or all of these diseases for many years — or indefinitely.32 But at least we know that with vaccines we can increase our odds of avoiding serious illness.
It may not be a perfect strategy, but it works.
Related content

Optum Rx Drug Pipeline Insights Reports

8 ways to make drugs more affordable

Empowering clients with more choice and transparency
Sources
- Frontiers in Immunology. Mind the "Vaccine Fatigue." Published March 10, 2022. Accessed September 8, 2023.
- Fortune. It’s not just you. Everyone really is sick this holiday season as the U.S. battles a ‘worst in a decade’ flu and rising COVID cases. Published December 20, 2022. Accessed August 28, 2023.
- Johns Hopkins Bloomberg School of Public Health. Preventing Another “Tripledemic” with Vaccines for Flu, COVID, and RSV. Published July 31, 2023. Accessed August 30, 2023.
- Fortune. Is the U.S. headed for another ‘tripledemic’ this fall? As COVID cases and hospitalizations rise, experts warn it could happen again. Published August 4, 2023. Accessed August 28, 2023.
- American Psychological Association. Social science and the COVID-19 vaccines. Published March 1, 2021. Accessed August 28, 2023.
- Psychology Today. Agency Is the Highest Level of Personal Competence. Published March 27, 2022. Accessed September 7, 2023.
- Preventing Chronic Disease. Relating Health Locus of Control to Health Care Use, Adherence, and Transition Readiness Among Youths With Chronic Conditions, North Carolina, 2015. Published online July 21, 2016. Accessed September 7, 2023.
- Frontiers in Psychology. What Is the Sense of Agency and Why Does it Matter? Published online August 29, 2016. Accessed September 7, 2023.
- Preventing Chronic Disease. Relating Health Locus of Control to Health Care Use, Adherence, and Transition Readiness Among Youths With Chronic Conditions, North Carolina, 2015. Published online July 21, 2016. Accessed September 7, 2023.
- Psychology Today. Agency Is the Highest Level of Personal Competence. Published March 27, 2022. Accessed September 7, 2023.
- Vaccines (Basel). Who Is Willing to Get Vaccinated? A Study into the Psychological, Socio-Demographic, and Cultural Determinants of COVID-19 Vaccination Intentions. Published online July 21, 2021. Accessed September 7, 2023.
- American Psychological Association. Social science and the COVID-19 vaccines. Published March 1, 2021. Accessed August 28, 2023.
- Ibid.
- Johns Hopkins Bloomberg School of Public Health. Preventing Another “Tripledemic” with Vaccines for Flu, COVID, and RSV. Published July 31, 2023. Accessed August 30, 2023.
- Frontiers in Microbiology. Impact of Vaccines; Health, Economic and Social Perspectives. Published July 14, 2020.
- La Presse Médicale. Life and death of smallpox. Published September 2022. Accessed September 6, 2023.
- World Health Organization. Vaccines and immunization. Accessed September 6, 2023.
- UCLA Health. The fastest vaccine in history. Published December 10, 2020.
- National Institutes of Health (NIH). COVID-19 Vaccination Communication: Applying Behavioral and Social Science to Address Vaccine Hesitancy and Foster Vaccine Confidence. Published December 2020. Accessed August 28, 2023.
- Vaccines (Basel). Who Is Willing to Get Vaccinated? A Study into the Psychological, Socio-Demographic, and Cultural Determinants of COVID-19 Vaccination Intentions. Published online July 21, 2021. Accessed September 7, 2023.
- Business and Society Review. Understanding the impact of pandemics on society with a special focus on COVID‐19. Published December 11, 2022.
- Frontiers in Microbiology. Impact of Vaccines; Health, Economic and Social Perspectives. Published July 14, 2020. Accessed August 30, 2023.
- National Institutes of Health (NIH). COVID-19 Vaccination Communication: Applying Behavioral and Social Science to Address Vaccine Hesitancy and Foster Vaccine Confidence. Published December 2020. Accessed August 28, 2023.
- Vaccines (Basel). Who Is Willing to Get Vaccinated? A Study into the Psychological, Socio-Demographic, and Cultural Determinants of COVID-19 Vaccination Intentions. Published online July 21, 2021. Accessed September 7, 2023.
- Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2019. Published December 2019. Accessed September 1, 2023.
- Pew Charitable Trusts. Federal Action Needed to Address Antibiotic Resistance in Older Americans. Published October 7, 2021. Accessed September 1, 2023.
- Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2019. Published December 2019. Accessed September 1, 2023.
- Health Affairs. The Social Value Of Vaccination Programs: Beyond Cost-Effectiveness. Published February 2016. Accessed August 24, 2023.
- Ibid.
- Cleveland Clinic. Virus. Last reviewed March 29, 2023. Accessed August 31, 2023.
- University of Texas at Austin Biodiversity Center. Viruses, biodiversity, and evolution. Published Friday, 24 April 2020. Accessed August 31, 2023.
- Harvard Medical School. Why do we need new flu shots every year? Published April 23, 2023. Accessed August 31, 2023.



