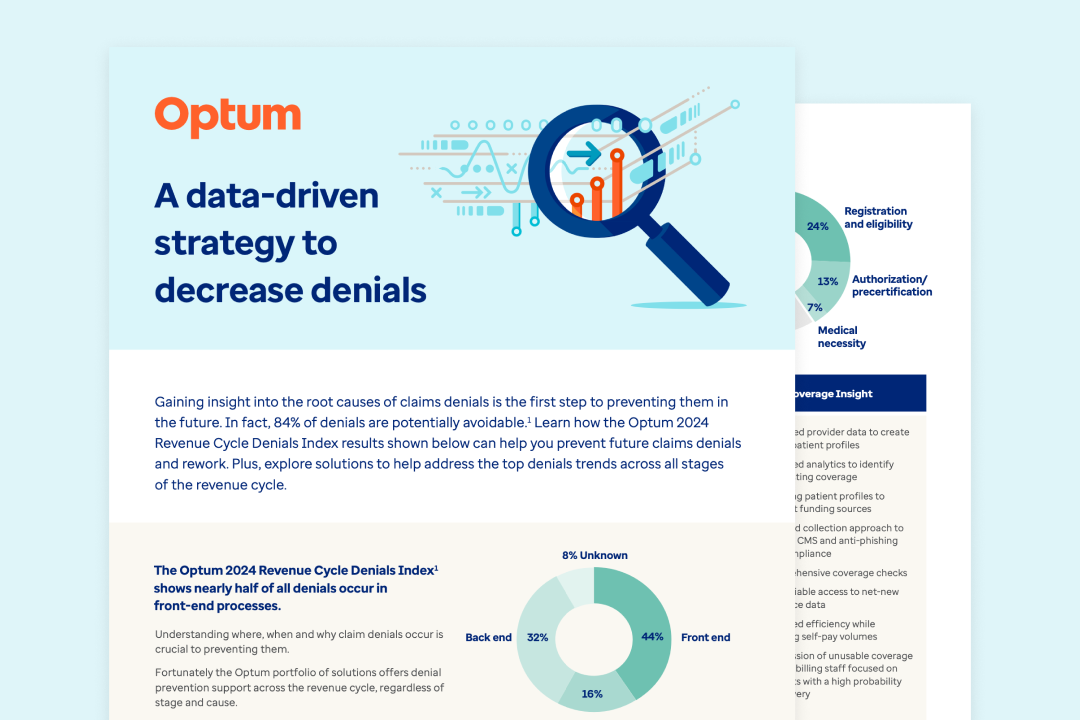
A recent study1 of more than 124 million medical claims from more than 1,400 hospitals nationwide found that claim denials are still increasing, with 84% being potentially avoidable.
Our 2024 strategy infographic offers insights and solutions to national claim denials pain points across each stage of the revenue cycle, including breakdowns of common root causes. Learn more about:
- Addressing registration and eligibility barriers to denial prevention
- Capabilities to evolve with increasingly complex patient care
- Clear understand of payer reimbursement rules
Complete the form to download the infographic.
- The Optum 2024 Revenue Cycle Denials Index is an internal analysis of approximately 124 million hospital claim remits valued at $500 billion in total charges across more than 1,400 U.S. hospitals.